Connect With Us
Blog
Items filtered by date: November 2024
Finding Relief for Cracked Heels

Cracked heels, also known as fissures, are a common foot condition where the skin on the heels becomes dry, thickened, and eventually splits. These cracks can be painful and, in severe cases, may lead to infection. The primary causes of cracked heels include dry skin, prolonged standing, excessive pressure on the feet, and wearing open-back shoes. To find relief, it is important to keep the feet moisturized with thick creams or ointments that help heal and hydrate the skin. Regular exfoliation with a pumice stone can remove dead skin and prevent the buildup that leads to cracks. Wearing comfortable, supportive shoes with proper cushioning can also reduce pressure on the heels. If you have developed persistent cracked heels, it is suggested that you consult a podiatrist who can offer prescribed medication for effective relief and treatment.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact David Williams, DPM from El Paso Feet. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our office located in El Paso, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Causes and Relief From Foot Blisters While Hiking

Foot blisters are a common nuisance for hikers, often caused by friction, moisture, and wearing poorly fitting footwear. When the skin rubs against shoes or socks, the top layer of skin can separate, leading to fluid-filled blisters. To prevent these painful injuries, selecting the right footwear is vital, as shoes should fit well and provide ample support. Choosing moisture-wicking socks can help keep feet dry, reducing friction and the likelihood of blisters. Additionally, applying blister prevention products, such as adhesive pads, can offer an extra layer of protection. It is also beneficial to gradually break in new shoes before embarking on long hikes to allow the feet to adjust. Foot blisters can easily deter hikers from partaking in long or short hikes. If you have developed a blister from hiking, it is suggested that you confer with a podiatrist who can offer you effective relief and prevention solutions.
Blisters may appear as a single bubble or in a cluster. They can cause a lot of pain and may be filled with pus, blood, or watery serum. If your feet are hurting, contact David Williams, DPM of El Paso Feet. Our doctor can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters are often the result of friction. This happens due to the constant rubbing from shoes, which can lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
Symptoms
(Blister symptoms may vary depending on what is causing them)
- Bubble of skin filled with fluid
- Redness
- Moderate to severe pain
- Itching
Prevention & Treatment
In order to prevent blisters, you should be sure to wear comfortable shoes with socks that cushion your feet and absorb sweat. Breaking a blister open may increase your chances of developing an infection. However, if your blister breaks, you should wash the area with soap and water immediately and then apply a bandage to the affected area. If your blisters cause severe pain it is important that you call your podiatrist right away.
If you have any questions, please feel free to contact our office located in El Paso, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Dangers of Peripheral Artery Disease
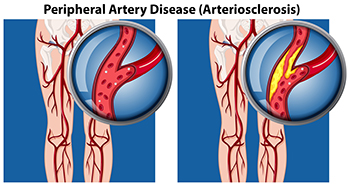
Peripheral artery disease, or PAD, occurs when blood flow to the feet and legs is restricted due to narrowed arteries. This condition can significantly impact the health of your feet. One of the primary symptoms of peripheral artery disease is muscle cramping or pain during physical activity, but it often affects the feet in more critical ways. People with PAD may notice that cuts, scrapes, or blisters on their feet are slow to heal. In fact, they may not heal at all. Prolonged inadequate blood flow can result in tissue damage, resulting in ulcers or even gangrene. Poor circulation caused by PAD also can lead to a decreased skin temperature in the feet, making one foot feel much colder than the other. Other visible signs include poor nail growth or the loss of hair on the toes and lower legs. A podiatrist can help to manage PAD by monitoring blood circulation in the feet and implementing treatment that enhances blood flow and promotes healing. If you have foot problems caused by peripheral artery disease, it is suggested that you schedule an appointment with a podiatrist for an exam and treatment.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with David Williams, DPM from El Paso Feet. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our office located in El Paso, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Three Phases of Diabetic Wound Healing

Diabetic foot wounds progress through three key phases, the inflammatory, proliferative, and maturation stages. The inflammatory phase is when the body initiates its immune response, removing debris and bacteria. In people with diabetes, this phase can be extended because of poor circulation and weakened immunity, which delay healing. The proliferative phase focuses on tissue repair, as new blood vessels form and collagen builds up to close the wound. Diabetic wounds may experience slow progress during this phase, which increases the risk of infection. The maturation phase involves the remodeling of tissue, which can sometimes extend beyond a year. A podiatrist plays a critical role in managing diabetic foot wounds by conducting regular exams and recommending advanced wound care treatment when necessary. If you have diabetic foot wounds, it is suggested that you are under the care of a podiatrist who can effectively treat this serious condition.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with David Williams, DPM from El Paso Feet. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in El Paso, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
