Connect With Us

Toenail Fungus
Toenail fungus is a frustrating problem that affects many people. It can be persistent and hard to get rid of. As many different types of fungi are present throughout the environment, it is very easy to contract toenail fungus.
The feet are especially susceptible to toenail fungus because shoes and socks create the ideal dark and moist environment that fungal infections thrive in. While fungal infections of the nail plate are quite common, if left untreated they can spread beyond the toenail and into the skin and other parts of the body.
Signs of toenail fungus include a thickened nail that has become yellow or brown in color, a foul smell, and debris beneath the nail. The toe may become painful due to the pressure of a thicker nail or the buildup of debris.
Treatment for toenail fungus is most effective during the early stages of an infection. If there is an accumulation of debris beneath the nail plate, an ingrown nail or a more serious infection can occur. While each treatment varies between patients, your podiatrist may prescribe you oral medications, topical liquids and creams, or laser therapy. To determine the best treatment process for you, be sure to visit your podiatrist at the first signs of toenail fungus.
Recognizing Signs of Diabetes in the Foot

Diabetes can manifest in the feet through several noticeable signs. One common symptom is persistent numbness or tingling, often caused by nerve damage, known as diabetic neuropathy. This condition can lead to a loss of sensation, making it difficult to detect injuries or infections. Another sign is slow-healing sores or ulcers, which can develop from minor cuts or blisters due to poor circulation. Discoloration of the skin, such as redness, can indicate inflammation or infection. Swelling in the feet and ankles might also be present, signaling potential underlying issues. Additionally, changes in skin texture, including dryness or cracking, can occur. Fungal infections, particularly between the toes, are more frequent in diabetics. If you have diabetes, it is strongly suggested that you are under the care of a podiatrist who can help you manage this serious condition.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact David Williams, DPM from El Paso Feet. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in El Paso, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How to Care for Diabetic Foot
Millions of people are affected by diabetes each year. Diabetes damages blood vessels in all parts of the body, especially the feet. The legs and feet may develop slow blood flow, which causes neuropathy, or nerve damage. Once a diabetic patient develops neuropathy, it is important that the feet are well taken care of. Otherwise, the lower limbs may have to be amputated. This only happens in drastic cases, but it shows how seriously diabetic foot care should be taken.
It is very important to always wash and dry the feet thoroughly, especially in between the toes, if you’re a diabetic. Secondly, examining your feet and toes for redness or sores must be done, even if you do not feel pain. You may also want to examine your feet from the bottom. Try to avoid wearing colored socks to prevent infections that may occur from the dye. Well-fitting socks are also highly recommended.
A diabetic’s physician should always monitor their blood levels to test how well blood sugars are being maintained. In addition to giving advice about everyday eating habits and foot care, a physician may prescribe medicine to help with the diabetic patient’s neuropathy. It is also advised to see a podiatrist if experiencing any feet conditions. Toenails may also need to be taken care of by a podiatrist. This prevents patients from cutting too deeply around their cuticles, which can lead to infection.
A person can take care of their feet at home by following the instructions of their physician. Using creams on one’s feet is also an effective way to heal dryness. Proceed with caution when using tools to remove calluses, as severe diabetics may not be able to feel pain on their feet. If any complications arise do not hesitate to contact a podiatrist.
On a daily basis, diabetic feet must be checked. If you are ever concerned about something, contact your health care professional. You never want to wait until a wound becomes too severe to treat. If left untreated, gangrene may develop. Gangrene is a serious infection that can lead to sepsis or amputation. It is also important for diabetics to be on the lookout for ulcers. Ulcers are sores that develop from tissue loss on the skin. They can be quite painful and require intensive treatment. Early treatment and everyday inspection are imperative to staying healthy.
Custom Orthotics For Outdoor Activity
Embrace the great outdoors with confidence and comfort! Whether you're hiking, jogging, or exploring nature, Custom Orthotics are your perfect companion. Tailored to your foot's unique needs, they provide stability on uneven terrains and cushioning for those longer adventures. Don't let foot discomfort limit your outdoor experiences. With Custom Orthotics, every step is supported and secure. Call today to schedule an appointment.
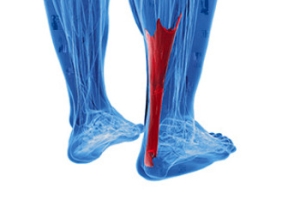
Achilles Tendon Ruptures in Sports Activities
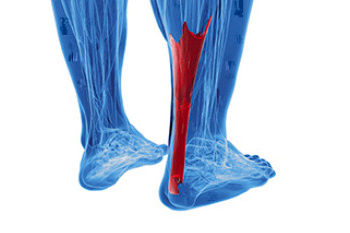
Achilles tendon ruptures are a significant injury that can often affecting athletes engaged in high-impact sports like basketball, soccer, and tennis. This injury happens when the tendon connecting the calf muscles to the heel bone tears, typically during a sudden acceleration, jump, or change in direction. The rupture results in immediate pain, swelling, and an inability to push off the foot or stand on tiptoe. Risk factors include inadequate warm-up, tight calf muscles, and previous tendonitis. Early diagnosis and treatment are important and may include surgical repair for optimal recovery. Preventative measures, such as regular stretching, strengthening exercises, and wearing appropriate footwear, can reduce the risk of an Achilles tendon rupture. If you have endured this type of injury, it is suggested that you schedule an appointment with a podiatrist who can successfully treat an Achilles tendon injury.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact David Williams, DPM of El Paso Feet. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in El Paso, TX . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Achilles Tendon Injuries
The Achilles tendon is the largest tendon in the body; it is a tough band of fibrous tissue that stretches from the bones of the heel to the calf muscles. This tendon is what allows us to stand on our toes while running, walking, or jumping, it is common for this tendon to become injured. In severe cases, the Achilles tendon may become partially torn or completely ruptured. However, this tendon is susceptible to injury because of its limited blood supply and the high level of tension it endures.
The people who are more likely to suffer from Achilles tendon injuries are athletes who partake in activities that require them to speed up, slow down, or pivot. Consequently, athletes who engage in running, gymnastics, dance, football, baseball, basketball, or tennis are more likely to suffer from Achilles tendon injuries. Additionally, there are other factors that may make you more prone to this injury. People who wear high heels, have flat feet, tight leg muscles or tendons, or take medicines called glucocorticoids are more likely to have Achilles tendon injuries.
A common symptom of an Achilles tendon injury is pain above the heel that is felt when you stand on your toes. However, if the tendon is ruptured, the pain will be severe, and the area may become swollen and stiff. Other symptoms may be reduced strength in the lower ankle or leg area, and reduced range of motion in the ankle. When the Achilles tendon tears, there is usually a popping sound that occurs along with it. People who have acute tears or ruptures may find walking and standing to be difficult.
If you suspect you have injured your Achilles tendon, you should see your podiatrist to have a physical examination. Your podiatrist will likely conduct a series of tests to diagnose your injury including a “calf-squeeze” test. Calf squeeze tests are performed by first squeezing the calf muscle on the healthy leg. This will pull on the tendon and consequently cause the foot to move. Afterward, the same test will be performed on the injured leg. If the tendon is torn, the foot won’t move because the calf muscle won’t be connected to the foot.
Custom Orthotics as Part of Treatment Plan for Plantar Fasciitis
 Custom-made orthotics are specifically designed shoe inserts tailored to an individual's unique foot structure and needs. They play a significant role in treating plantar fasciitis, a common condition caused by inflammation of the plantar fascia, a thick band of tissue connecting the heel bone to the toes, causing heel pain. These orthotics provide targeted support and cushioning, helping to redistribute pressure across the feet, reduce strain on the plantar fascia, and correct abnormal foot mechanics that contribute to the condition. By improving alignment and stability, custom orthotics can alleviate pain, enhance comfort, and promote healing as part of a comprehensive treatment program. In addition to wearing orthotics, treatment for plantar fasciitis may include stretching exercises, anti-inflammatory medications, and proper footwear. Consistent use of orthotics can prevent recurrence and provide long-term relief. If you suffer from plantar fasciitis, it is suggested that you consult a podiatrist who can design orthotics suited to your specific needs.
Custom-made orthotics are specifically designed shoe inserts tailored to an individual's unique foot structure and needs. They play a significant role in treating plantar fasciitis, a common condition caused by inflammation of the plantar fascia, a thick band of tissue connecting the heel bone to the toes, causing heel pain. These orthotics provide targeted support and cushioning, helping to redistribute pressure across the feet, reduce strain on the plantar fascia, and correct abnormal foot mechanics that contribute to the condition. By improving alignment and stability, custom orthotics can alleviate pain, enhance comfort, and promote healing as part of a comprehensive treatment program. In addition to wearing orthotics, treatment for plantar fasciitis may include stretching exercises, anti-inflammatory medications, and proper footwear. Consistent use of orthotics can prevent recurrence and provide long-term relief. If you suffer from plantar fasciitis, it is suggested that you consult a podiatrist who can design orthotics suited to your specific needs.
Custom orthotics and shoe inserts are not just for cushioning the soles; they are about supporting the foundation of our body - our feet. The advantages extend far beyond immediate relief from discomfort. These personalized solutions, that Our doctor can prescribe, can significantly impact a person’s posture, alleviate pain in various parts of the body, and even enhance athletic performance.
As we lace up our shoes each day, having the right support can make a world of difference. Custom orthotics are like tailored suites for our feet, offering a bespoke solution to address our unique biomechanical needs. They provide stability where it is lacking, correct imbalances, and ensure that every step is a confident and pain-free one.
Custom orthotics and shoe inserts offer long-term health benefits. By addressing issues such as overpronation or underpronation, heel pain, plantar fasciitis, etc. orthotics can help prevent injuries and mitigate the progression of existing conditions. It’s an investment not just in the present, but in the future health of your feet and consequently, your overall well-being.
If you have any questions please contact our office located in El Paso, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Investing in Custom Orthotics Means Investing in Foot Health
Custom orthotics offer a tailored approach to foot health, providing a host of benefits that extend far beyond conventional shoe inserts. One of the primary advantages lies in their ability to address specific biomechanical issues. Unlike off-the-shelf inserts, custom orthotics are crafted based on an individual's unique foot structure, gait, and any existing foot conditions.
The personalized design of custom orthotics ensures optimal support for the arches, promoting proper alignment and distributing pressure evenly across the feet. This can be particularly beneficial for individuals dealing with issues such as overpronation or underpronation, as custom orthotics help correct imbalances that may lead to discomfort or injury.
Beyond biomechanics, custom orthotics can alleviate a range of foot problems, including plantar fasciitis, bunions, and metatarsalgia. They provide targeted relief to areas under stress, reducing pain and inflammation. Additionally, for those with specific medical conditions like diabetes, custom orthotics can play a crucial role in preventing complications associated with poor foot health.
Comfort is another key aspect of custom orthotics. By accommodating the unique contours of an individual's feet, these inserts enhance overall comfort, making daily activities more enjoyable. Whether for athletes looking to optimize performance or individuals seeking relief from chronic foot pain, custom orthotics offer a versatile solution.
Investing in custom orthotics is an investment in long-term foot health. They not only provide immediate relief but also contribute to the prevention of future issues. With the ability to seamlessly integrate into various types of footwear, custom orthotics empower individuals to prioritize foot comfort without compromising on style. In essence, custom orthotics are a personalized prescription for happy, healthy, and pain-free feet.
Painful Bunions? There's a New Treatment Option in Lapiplasty®
Foot Blisters on Elderly Feet
 Blistering skin lesions on the feet of the elderly can be a common and concerning issue. These lesions, often filled with fluid, can result from various factors, including friction, pressure, and decreased skin integrity associated with aging. The skin of elderly individuals tends to become thinner, drier, and more fragile over time, making it more susceptible to damage and blister formation. Moreover, age-related conditions such as diabetes and reduced mobility add to the risk of blistering skin lesions. Diabetic neuropathy can lead to decreased sensation in the feet, making it harder for individuals to detect and address issues like friction and pressure points, which can eventually lead to blisters. If left untreated, blistering skin lesions can increase the risk of infection and other complications, particularly in elderly individuals with compromised immune systems. If you are elderly and experiencing such blisters, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment.
Blistering skin lesions on the feet of the elderly can be a common and concerning issue. These lesions, often filled with fluid, can result from various factors, including friction, pressure, and decreased skin integrity associated with aging. The skin of elderly individuals tends to become thinner, drier, and more fragile over time, making it more susceptible to damage and blister formation. Moreover, age-related conditions such as diabetes and reduced mobility add to the risk of blistering skin lesions. Diabetic neuropathy can lead to decreased sensation in the feet, making it harder for individuals to detect and address issues like friction and pressure points, which can eventually lead to blisters. If left untreated, blistering skin lesions can increase the risk of infection and other complications, particularly in elderly individuals with compromised immune systems. If you are elderly and experiencing such blisters, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment.
Blisters are prone to making everyday activities extremely uncomfortable. If your feet are hurting, contact David Williams, DPM of El Paso Feet. Our doctor can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters develop as a result of constantly wearing tight or ill-fitting footwear. This happens due to the constant rubbing from the shoe, which can often lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
How Do Blisters Form?
Blisters on the feet are often the result of constant friction of skin and material, usually by shoe rubbing. Walking in sandals, boots, or shoes that don’t fit properly for long periods of time can result in a blister. Having consistent foot moisture and humidity can easily lead to blister formation.
Prevention & Treatment
It is important to properly care for the affected area in order to prevent infection and ease the pain. Do not lance the blister and use a Band-Aid to provide pain relief. Also, be sure to keep your feet dry and wear proper fitting shoes. If you see blood or pus in a blister, seek assistance from a podiatrist.
If you have any questions, please feel free to contact our office located in El Paso, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.